Digital Health in Low-Resource Settings: What Works and What Doesn’t
- Prishita Vora
- Sep 2
- 1 min read
Updated: Sep 12
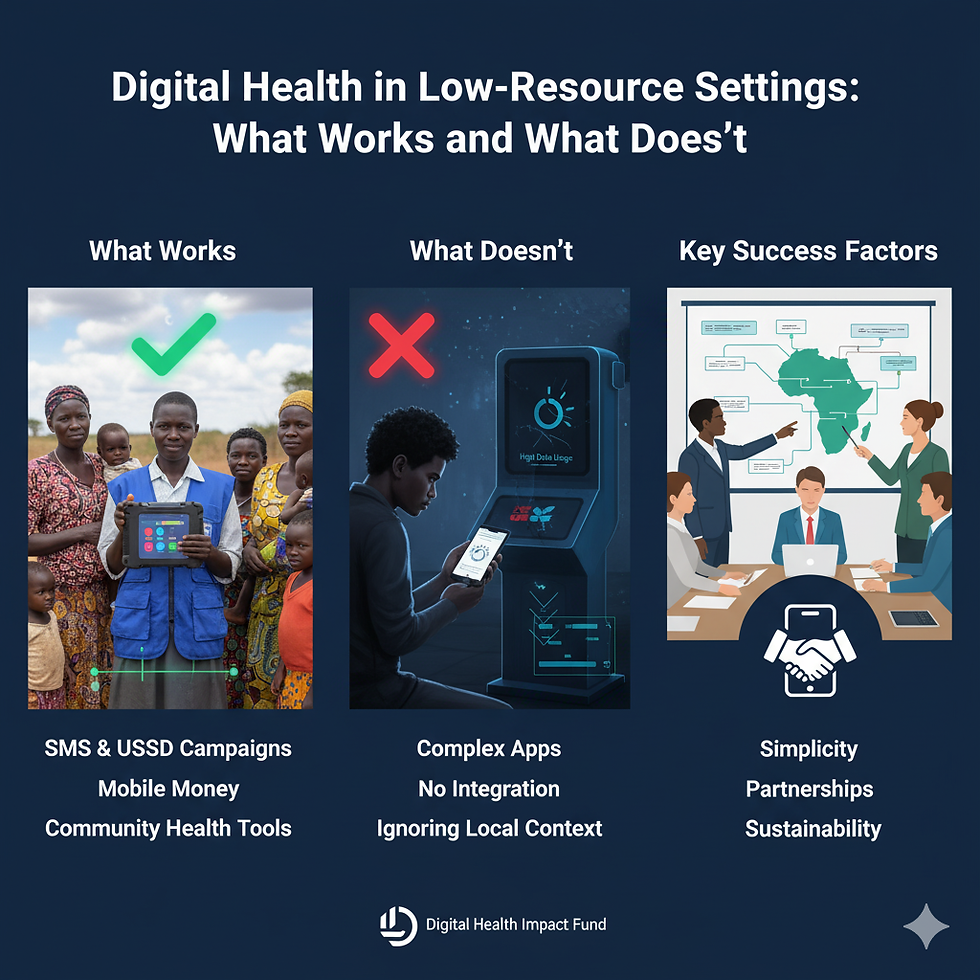
Digital health has been heralded as a game-changer for low- and middle-income countries. With high mobile penetration but low access to health facilities, Africa and Asia are prime markets for digital health solutions. Yet, while some initiatives have thrived, others have failed. What lessons can we learn?
1. What Works
SMS & USSD Campaigns: Simple tools like SMS reminders for vaccinations or antenatal care have proven highly effective in countries like Kenya and Tanzania (WHO, 2018).
Mobile Money Integration: Linking mobile health services with payment platforms like M-PESA ensures affordability and convenience.
Community Health Worker Tools: Equipping front line workers with digital tablets for data collection and teleconsultation increases efficiency and accuracy.
2. What Doesn’t
Overly Complex Apps: Many pilots failed because they required high data use or advanced devices not available to low-income users.
Lack of Integration: Standalone apps that don’t link to national health systems often fizzle out after donor funding ends.
Ignoring Local Context: Imported solutions that don’t adapt to cultural and linguistic realities struggle to gain traction.
3. Key Success Factors
Simplicity: The best tools are user-friendly and low-cost.
Partnerships: Success depends on aligning with ministries, NGOs, and telecom companies.
Sustainability: Solutions must outlast donor cycles through viable business models.
Digital health can transform access in low-resource settings—but only when solutions are simple, integrated, context-specific, and sustainable. Innovation must serve communities, not just technology trends.
References
WHO. (2018). Digital Health Atlas: Lessons from Africa.
World Bank. (2020). Digital Health in Low- and Middle-Income Countries.
GSMA. (2022). Mobile for Development in Africa.



Comments